Scientists at the Hebrew University of Jerusalem have succeeded in reversing brain birth defects in animal models, using stem cells to replace defective brain cells. The work of Prof. Joseph Yanai and his associates at the Hebrew University-Hadassah Medical School was presented at the Tel Aviv Stem Cells Conference last spring and is expected to be presented and published nest year at the seventh annual meeting of the International Society for Stem Cell Research in Barcelona, Spain.
Involved in the project with Prof. Yanai are Prof. Tamir Ben-Hur, head of the Department of Neurology at the Hebrew University-Hadassah Medical School, and his group, as well as Prof. Ted Slotkin at Duke University in North Carolina, where Prof. Yanai is an adjunct professor.

Neural and behavioral birth defects, such as learning disabilities, are particularly difficult to treat, compared to defects with known cause factors such as Parkinson’s or Alzheimer’s disease, because the prenatal teratogen – the substances that cause the abnormalities — act diffusely in the fetal brain, resulting in multiple defects.
Prof. Yanai and his associates were able to overcome this obstacle in laboratory tests with mice by using mouse embryonic neural stem cells. These cells migrate in the brain, search for the deficiency that caused the defect, and then differentiate into becoming the cells needed to repair the damage.
Generally speaking, stem cells may develop into any type of cell in the body, however at a certain point they begin to commit to a general function, such as neural stem cells, destined to play a role in the brain/ nervous system. At more advanced developmental stages, the neural stem cells take on an even more specific role as neural or glial (supporting) cells within the brain/ nervous system.
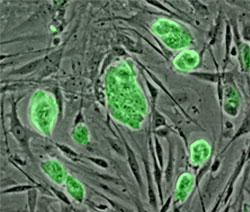
In the researchers’ animal model, they were able to reverse learning deficits in the offspring of pregnant mice who were exposed to organophosphate (a pesticide) and heroin. This was done by direct neural stem cell transplantation into the brains of the offspring. The recovery was almost one hundred percent, as proved in behavioral tests in which the treated animals improved to normal behavior and learning scores after the transplantation. On the molecular level, brain chemistry of the treated animals was also restored to normal.
The researchers went one step further. Puzzled by the stem cells’ ability to work even in those cases where most of them died out in the host brain, the scientists went on to discover that the neural stem cells succeed before they die in inducing the host brain itself to produce large number of stem cells which repair the damage. This discovery, finally settling a major question in stem cell research, evoked great interest and was published earlier this year in one of the leading journals in the field, Molecular Psychiatry.
The scientists are now in the midst of developing procedures for the least invasive method for administering the neural stem cells, which is probably via blood vessels, thus making the therapy practical and clinically feasible.
Normally, stem cells are derived from individuals genetically different from the patient to be transplanted, and therefore the efficacy of the treatment suffers from immunological rejection. For this reason, another important avenue of the ongoing study, toward the same goals, will be to eliminate the immunological rejection of the transplant, which will become possible by taking cells from the patient’s own body — from a place where they are easily obtained — by manipulating them to return to their stem cell phase of development, and then transplanting them into the patient’s brain via the blood stream. One important advantage of this approach will be to eliminate the controversial ethical issues involved in the use of embryo stem cells.
The research on the project has been supported by the US National Institutes of Health, the US-Israel Binational Science Foundation and the Israel anti-drug authorities.