(Photo: Tomer Yaffe)
Heart disease is a well-known killer. Just one decade ago, the WHO (World Health Organization) released its findings showing that heart disease has become a global epidemic with approximately 17 million people dying each year from heart attack and stroke; at the time of publishing, this made up nearly one-third of deaths globally; and the WHO then prospected that this number would only rise with time. Thankfully, medical research has produced some significant advances to combat this medical threat and continues to develop innovative methods to treat and prevent heart disease. Not surprisingly, a number of these advances (and ongoing research) are coming from none other than Israel. IsraCast went to Shaare Zedek Medical Hospital to learn more.
LISTEN TO THE INTERVIEW WITH DR. BALKIN:
This journey brought us to Shaare Zedek’s Cardiology ward on the 10th floor of the Jerusalem-based hospital, where the first thing that meets you as you step out of the elevator is a giant poster depicting a life-sized cigarette being snuffed out. So all lingering doubts can now be put to rest – yes, smoking is strongly correlated to heart disease!
In the ICCU (Intensive Coronary Care Unit)
The ICCU has changed from post-trauma treatment, to actively halting and preventing coronary damage.
Upon our arrival, we were greeted with a warm welcome and disarmingly kind smile by Dr. Jonathan Balkin. You wouldn’t know it from his pleasant demeanor and nonchalant South African accent, but as director of Shaare Zedek Hospital’s ICCU (Intensive Coronary Care Unit), this man clearly has nerves of steel. The ICCU is responsible for patients at what is most often their most critical and acute state – it oversees the initial acute care and diagnosis of patients that arrive to the cardiology unit.
Doctor Balkin explained to IsraCast the critical role the ICCU plays today and how it has changed from post-trauma treatment, to actively halting and preventing coronary damage.
If in the past coronary care units used to treat patients after heart attacks and just monitor them and try to prevent arrhythmias, today coronary care units have become very, very involved in actively treating and reducing the size of heart attacks when patients are admitted. When a patient has a heart attack it’s usually due to blockage of an artery taking blood to the heart, and as a result the heart starts to die in a very quick fashion – after several hours the muscle of the heart is totally destroyed. So, we have a very short window of time in order to try and stop the process and to preserve as much muscle of the heart as possible. So, when a patient comes … we immediately call our team … and we take these patients directly to the cath lab and perform a cardiac catheterization.
Cardiac catheterization
Cardiac catheterization has been around for the last fifty odd years. Initially it was performed in patients with heart disease; in the 60’s and 70’s most of the patients with severe coronary disease had to undergo bypass surgery. Over the last few decades there have been many advances in the cath lab allowing diagnosis and treatment to now be simultaneously accomplished.
Over the last few decades there have been many advances in the cath lab allowing diagnosis and treatment to now be simultaneously accomplished.
Almost all patients in Israel who experience an acute heart attack undergo cardiac catheterization and percutaneous cardiac intervention in order to treat the critical lesion which has caused the acute symptoms. According to Dr. Balkin, more than half are patients who have acute coronary syndrome – in other words, they have something that’s occurred, starting in the days or weeks leading up to their admission, and urgently need to undergo cardiac catheterization. The other 40% of patients with coronary disease who undergo catheterization are patients who have stable symptoms and who are seen by their doctors, and because of the symptoms are directed to perform an elective procedure which, depending on the findings, can often be treated on the spot in the cath lab. Today approximately 80-85% of cardiac patients are treated in the cath lab, whereas twenty years ago, approximately 70-80% percent of patients would be transferred to the cardiac surgery department. This change of course offers a much quicker and convenient surgery for any patient to undergo, which allows them to be quickly treated, and quite possibly leave the hospital the following day; as opposed to the long and difficult recovery from open heart surgery, not to mention the many risks involved in the surgery itself and that fact that some patients are not physically able to undergo open heart surgery.
 Much of the stent technology used today in cardiac procedures are Israeli inventions – for instance, the B-stent (a balloon expandable stent which stays in the artery permanently improving blood flow to the artery and relieving chest pain), InStent, Medinol, Angiosonics Inc. (a catheter-delivered ultrasound for thrombolysis, a non-invasive therapeutic ultrasound in the heart – early studies have shown that it could break up clots in peripheral vessels), and Laser Industries (a Sharplan holmium/yag laser for unblocking multiply-occluded coronary vessels), as well as different diagnostic cardiology tools. It is worth noting that the official stance on such lifesaving inventions from the BDS (the Boycott, Divestment, and Sanctions movement which seeks to put economic and political pressure on Israel) movement is:
Much of the stent technology used today in cardiac procedures are Israeli inventions – for instance, the B-stent (a balloon expandable stent which stays in the artery permanently improving blood flow to the artery and relieving chest pain), InStent, Medinol, Angiosonics Inc. (a catheter-delivered ultrasound for thrombolysis, a non-invasive therapeutic ultrasound in the heart – early studies have shown that it could break up clots in peripheral vessels), and Laser Industries (a Sharplan holmium/yag laser for unblocking multiply-occluded coronary vessels), as well as different diagnostic cardiology tools. It is worth noting that the official stance on such lifesaving inventions from the BDS (the Boycott, Divestment, and Sanctions movement which seeks to put economic and political pressure on Israel) movement is:
Preferably before an emergency situation (whereby your judgment may be clouded by urgency and the optimum medical response) please inform your Cardiologist to ensure that a Balloon Expandable Stent is NEVER used. Request open heart surgery!
The critical first hours
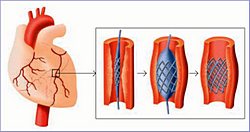 Cardiac Catheterizations are done in the initial minutes and hours after the patient reaches the unit. A percutaneous coronary intervention (coronary angioplasty with stent) allows the surgeons to identify the blocked artery, open it (often with a balloon) and place a stent (which is like a metal scaffolding) in the place of blockage to keep the artery open and restore blood flow. This limits the amount of damage as much as possible. Afterwards the patient is transferred to the coronary care unit where he/she is monitored for the next day or two. This initial treatment is key for the beginning of rehabilitation. Balkin told IsraCast, “During this time we very actively treat the patient – we assess the amount of damage that has occurred, and if the patient, for example, has heart failure, we will give him appropriate drugs. We will also give him drugs to prevent further heart attacks from occurring, which he will start immediately upon admission, and medicines which will prevent further damage from taking place (such as expansion of the heart and heart failure).”
Cardiac Catheterizations are done in the initial minutes and hours after the patient reaches the unit. A percutaneous coronary intervention (coronary angioplasty with stent) allows the surgeons to identify the blocked artery, open it (often with a balloon) and place a stent (which is like a metal scaffolding) in the place of blockage to keep the artery open and restore blood flow. This limits the amount of damage as much as possible. Afterwards the patient is transferred to the coronary care unit where he/she is monitored for the next day or two. This initial treatment is key for the beginning of rehabilitation. Balkin told IsraCast, “During this time we very actively treat the patient – we assess the amount of damage that has occurred, and if the patient, for example, has heart failure, we will give him appropriate drugs. We will also give him drugs to prevent further heart attacks from occurring, which he will start immediately upon admission, and medicines which will prevent further damage from taking place (such as expansion of the heart and heart failure).”
Heal your heart
The medical team at the ICCU must also help the patients deal with the shock of what has happened and begin to work through it.
However, despite their importance, acute care does not begin and end with procedures and medications. The medical team at the ICCU must also help the patients process the shock of what has happened and begin to work through it. “For many patients this is a devastating event. Most of these patients are in their young/middle ages, they feel perfectly healthy, and then they are struck down by a disease which is life-threatening and threatens to destroy their personal lives, their careers, and all their functions.” Doctor Balkin added, “So we need to act in ways to reassure them that they will be able to continue doing what they’ve done until now, often with the aid of medicines, and also to advise them to change their lifestyles to prevent further attacks from occurring.”
In addition, the families of the patients are often in need of help and support. According to Dr. Balkin, the patient is frequently the major bread winner or the leader of the family, and suddenly this strong, central figure is now in a situation where he/she is dependent upon other people. “People then have to change their roles a little bit, and we need to provide support, to reassure the family the patient will be able to get back to what he/she was doing before, and to try and encourage them also and make the lifestyle changes necessary to enable everybody to get back into a good and healthy lifestyle after their hospitalization.”
A long-term plan of action

Perhaps one of the most important factors in long-term rehabilitation for cardiac patients is to implement and maintain necessary lifestyle changes after their cardiac event. That is why Shaare Zedek manages a very successful cardiac rehabilitation program for their patients right on the cardiac floor. The Shaare Zedek Cardiac Rehabilitation Center is one of the leading rehabilitation centers in Israel. Headed by Dr. Yaakov Klein, it has been active now for over twenty-five years, and continues to grow.
After patients are admitted with a heart attack we almost automatically advise that they take part in a rehab program. And this rehab program usually runs for about three months, where the patients come twice or thrice weekly and they have a directed and controlled exercise program together with dietary and lifestyle advice, and to help them to get into living a healthy lifestyle.” Dr. Balkin explained to IsraCast, “Many of the patients have never done any exercise before. We think that exercise is an important component of the treatment and prevention of further heart disease, so we encourage all our patients to participate in the rehab program. And they enjoy it very much – for many of them it’s also a good social experience, and they get a lot of understanding about the [heart] disease, and I think they then face life with much more confidence.
Many patients fear exercise after the scare of a cardiac event, however, Dr. Balkin was quick to clarify that those fears are often exaggerated, as exercise is proven to have a manifold impact on the improved health of people with heart disease: from improved circulation to the heart and muscles, reducing the energy in demand on the heart, to helping control risk factors like angina and high blood pressure, and even combat depression, a common side effect of any serious illness. Balkin added that while it is true that someone who has severe heart disease and suddenly decides to exercise may have an event, and of course anyone middle-aged who decides to embark on an exercise program should do so carefully and gradually, and at least initially, should probably have some kind of medical assessment before starting an exercise program, overall, exercise is a very important part of therapy for patients with heart disease.
Technological advances in the cath lab

Shaare Zedek was founded over a century ago and has grown from a small community hospital to a major hospital in Israel today; and it has been on the forefront of applying new technology, particularly in the cardio catheterization laboratory, pioneering the use of artificial valves (a technology developed in Israel) which allows surgeons to place artificial valves in the heart through only a small hole in the leg, as opposed to performing open heart surgery. This specific program was started less than a decade ago and has now been used to successfully treat nearly 300 patients who have had their aortic valve changed during catheterization. This number includes a large number of patients who due to age, frailty, or additional medical conditions were deemed inoperable or at high risk for open heart surgery.
Dr. Balkin and his colleagues have played a significant role in introducing and promoting in Shaare Zedek, and in Israel, a new technology whereby both the left and right sides of the heart can be paced.
Dr. Balkin and his colleagues have played a significant role in introducing and promoting in Shaare Zedek, and in Israel, a new technology whereby both the left and right sides of the heart can be paced. This is particularly crucial for certain heart failure patients who have major deficiencies in the contraction of the heart which is significantly improved by the special pace maker which restores the wave of the heart contractions. This procedure has successfully helped patients with class 3-4 heart failure return to a state of improved health, mobility, and restored independence.
Shaare Zedek is also involved in applying a corrective procedure in the cath lab for patients with mitral valve disease which allows surgeons to attach a clip onto the mitral valve, which lessens the degree of leakage of the valve.
High expectations for the future of heart care
Without a doubt the advances in medicine in recent years have been dramatic for coronary care, both in drug therapy (specifically for high blood pressure and cholesterol) and in surgical procedures. They have also played a key role increasing longevity and improving the quality of those years for heart patients the world over. In the future, with improved technology, we may be able to prevent the onset of many diseases. Dr. Balkin speculated that the direction medicine is taking us right now will one day give us the genetic understanding to prevent the different types of heart disease that we deal with today. In fact, we are already seeing today that the diagnosis of many conditions can be made prenatally, and sometimes even treated, allowing for normal development and a normal lifestyle for the infant. Such in-utero procedures are already being successfully practiced in certain centers in Europe. Dr Balkin stated,
We live in a society where the value of life is placed very, very high, where for many couples, whether it’s for cultural or religious beliefs, terminating a pregnancy is something which is done reluctantly or not at all, and if we can offer (and hopefully in the future we’ll be able to offer) to many of these people solutions to congenital conditions which can be diagnosed and treated, I think it can make a big difference to society and the well-being of many people.
Out of Africa
With such advances already being practiced and eagerly developed in Israel, it is no wonder that Israel is number 28 in the World Health Organization’s latest ranking of the world’s health systems (which included 190 nations), beating Canada (ranked 30) and the United States (ranked 37). It’s hard to believe how far Israel has come as a nation in such a short span of time. Dr. Balkin however, remembers quite well, having himself made Aliyah (immigrated to Israel) as a young, newly married doctor nearly forty years ago.

(Photo: Tomer Yaffe)
Jonathan Balkin hails from a family of doctors, with both his father and grandfather being highly respected physicians of their time in South Africa. In his own words, “If I had chosen, I probably would have had a much easier career path if I’d stayed in South Africa because my family was a very well-known family, both in the medical community and also in the Jewish community. However, I am Zionist and I was encouraged to be a Zionist, probably almost from birth. My grandmother was a member of the Women’s Zionist League in South Africa, she was on WIZO, the world’s Women’s Zionist Organization; she’d already been to Palestine in 1935 as a delegate for WIZO, which, when you consider the situation of South Africa at that time, was really a major achievement and a major undertaking – going by boat, there were no airplanes in those days and it took about six weeks just to get to Palestine at that time and back. So I was brought up in a very Zionistic influence, and I joined Bnei Akiva as a young lad; that had a tremendous influence upon me and upon my outlook, and I’d already decided during my studies that I wanted to make my life in Israel. And I educated both in the Tnuah (movement) of Bnei Akiva amongst my peers, and we had a very, very strong leaning and yearning to come on Aliyah. And I got married to my wife, Terri, before we came on Aliyah, and as soon as I qualified, we came to Israel.
It was a very exciting time, also a very difficult time as you might imagine, the standards of medicine were very different from what I was used to in South Africa. The lifestyle in Israel was very, very different from what I’d experienced in South Africa, where at that time living in South Africa was like living in paradise for many, many people – it was very easy, and easy professionally, easy socially, easy financially. And to come to Israel at that time was a real challenge. But when you’re young you can do these things, and so I am very pleased that I did it.
Obviously the situation in South Africa has changed completely since I lived there, and I think today Israel is a very, very attractive country to want to live in. I think there are many people all over the world who would envy very much our lifestyle, I think they would envy very much our economy; I think they would envy even more our healthcare, which I think is one of the finest in the world, applied to everyone of all races; and it’s really been a privilege and a pleasure to be able to participate somewhat in the development of that medical knowledge and treatment which has transformed Israel over the last thirty years, obviously building on those tremendous pioneers who were here before us and set up the basic institutions, including mine (Shaare Zedek).
Heart disease and the Western world
According to Balkin, heart disease is on a rapid incline in developing countries such as China and former Soviet blocs. This is partly due to improved diagnosis and partly due to the lifestyle changes associated in the westernization of these countries – a more intensive and active economy causing high stress levels, and changes in eating habits. In other countries where people are very aware of their health, there is possibly some decline in heart disease. Certainly in the West there has been a decline in the mortality from heart disease, but this is likely due to the improved treatment which now allows people to live much longer than it was able to just a few decades ago.
Patients from near and far

Israel had indeed come a long way since the early days of the nation. In fact, today Israel is even a destination for medical tourism, where people come specifically to receive medical treatment, particularly from Eastern European countries. The cardiology and surgical departments at Shaare Zedek continuously see such patients who feel more secure with the standard of care in Israel than in their home countries. Of course, such care is expensive to do internationally, and is done mostly by the wealthy who can afford it, but Israel also has programs specifically geared to help those in underprivileged countries.
…a very high percent of our patients come from the Palestinian Authority and I’m sure that we do a tremendous amount to improve their care and lives as well.
One such program is the “Save a Heart Foundation”, located at the Wolfson Hospital in Jerusalem, where life-saving heart operations are performed on children from underprivileged nations (including Iraq, Syria, and Jordan), who would certainly not receive such care otherwise. In addition, many of the patients treated at Shaare Zedek come from the surrounding countries, including Israel’s Palestinian neighbors, according to Dr. Balkin, who stated, “Like all other patients, I will tell you that a very high percent of our patients come from the Palestinian Authority and I’m sure that we do a tremendous amount to improve their care and lives as well.”